|
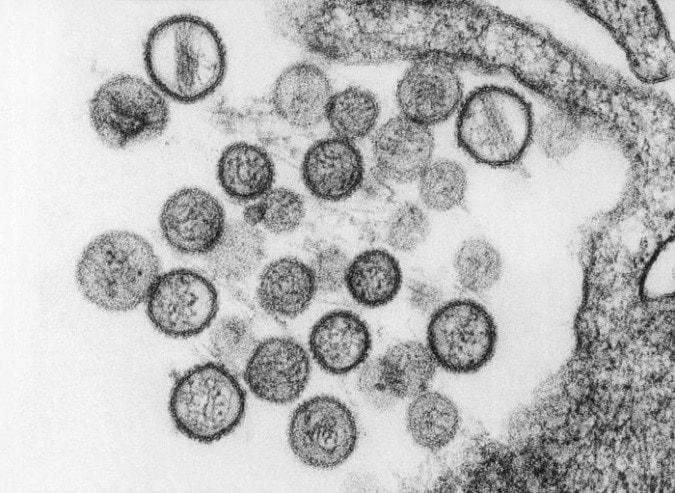
by Houssem Djeridi What are hantaviruses?Hantaviruses are a group of viruses that may be carried by some rodents. Some hantaviruses can cause a rare but deadly disease called hantavirus pulmonary syndrome (HPS). the related illness Hemorrhagic Fever with Renal Syndrome (HFRS) are rare infections caused by viruses belonging to the Bunyaviridae family. Viruses causing HPS are found in the Americas while those causing HFRS exist worldwide. Hantaviruses (genus Hantavirus, family Bunyaviridae) are a group of antigenically distinct RNA viruses carried in rodents and insectivores (shrews and moles). Each hantavirus is endemic in one, or at most, a few specific rodent or insectivore hosts, to which it is well adapted. At least 20 hantaviruses have been identified but estimates of the exact number of viruses vary. Newly identified hantaviruses are often named for the location where the virus is found; however, some of these viruses are later reclassified. Which rodents can cause humans to get Hantavirus ?Not all rodents carry hantavirus and there is usually no way to tell when a rodent has the virus. So, it is wise to avoid all contact with rodents when possible. Rodents, insectivores and bats known reservoir hosts for hantaviruses include rodents, insectivores (e.g., shrews and moles) and bats. Each virus is thought to be adapted to one or a few species, but spillover rodent, insectivore and bat hosts may not be unusual. Members of the mouse genus Apodemus carry Hantaan, Amur-Soochong and Dobrava-Belgrade viruses. Norway rats (Rattus norvegicus) are important reservoir hosts for Seoul virus; however, this virus has also been found in other species of rats including R. rattus (black rats), R. flavipectus, R. losea and R. nitidus. Bandicoot rats (Bandicota indica) carry Thailand virus, and bank voles (Myodes glareolus) are the reservoir hosts for Puumala virus. Tula virus has been found in several species of voles in the genus Microtus, in the water vole Arvicola amphibius and in the steppe lemming (Lagurus lagurus). Deer mice (Peromyscus maniculatus) carry Sin Nombre virus,while Black Creek Canal and Muleshoe viruses have been found in cotton rats (Sigmodon hispidus). Andes virus and its variants occur in rodents belonging to the South American mousegenera Akodon and Necromys and the rice rat genus Oligoryzomys. Laguna Negra virus has been detected in the vesper mice Calomys laucha and Calomys callidus, while Rio Mamore infects members of Oligoryzomys. Transmission
SymptomsHemorrhagic Fever with Renal Syndrome HFRS
Hantavirus Pulmonary Syndrome HP
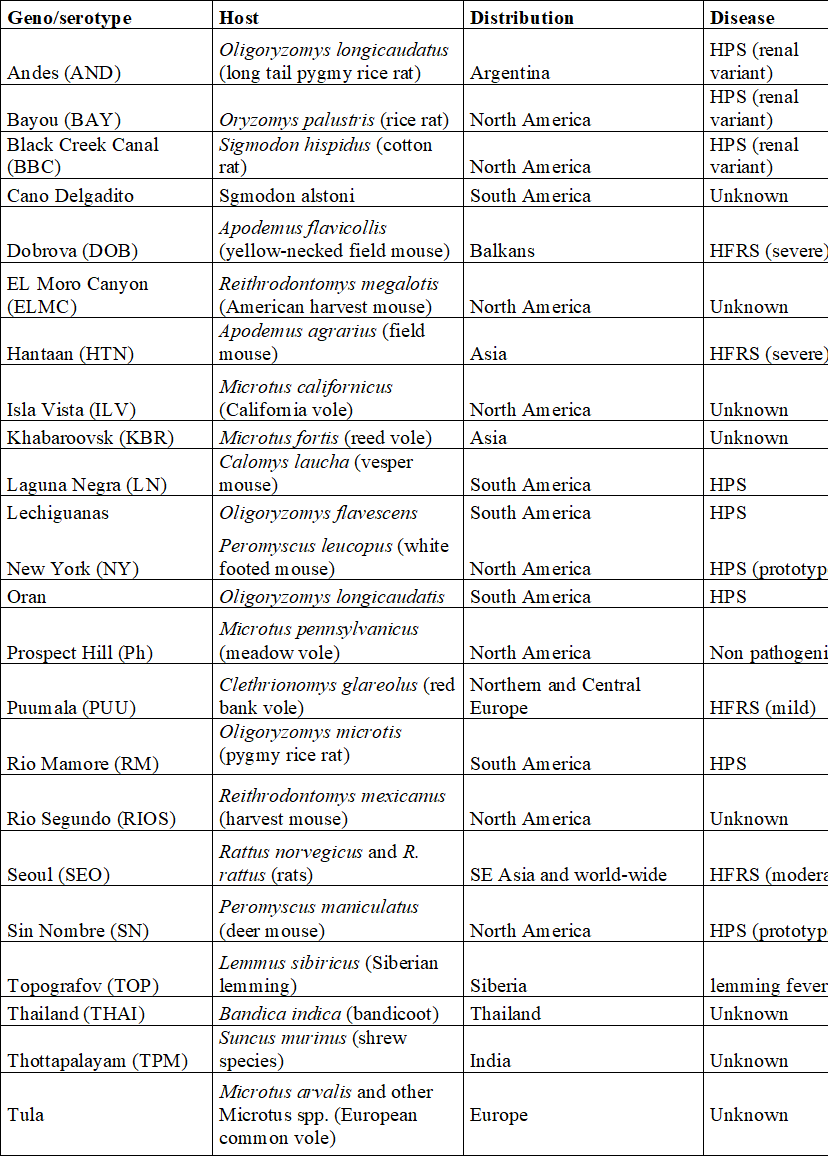
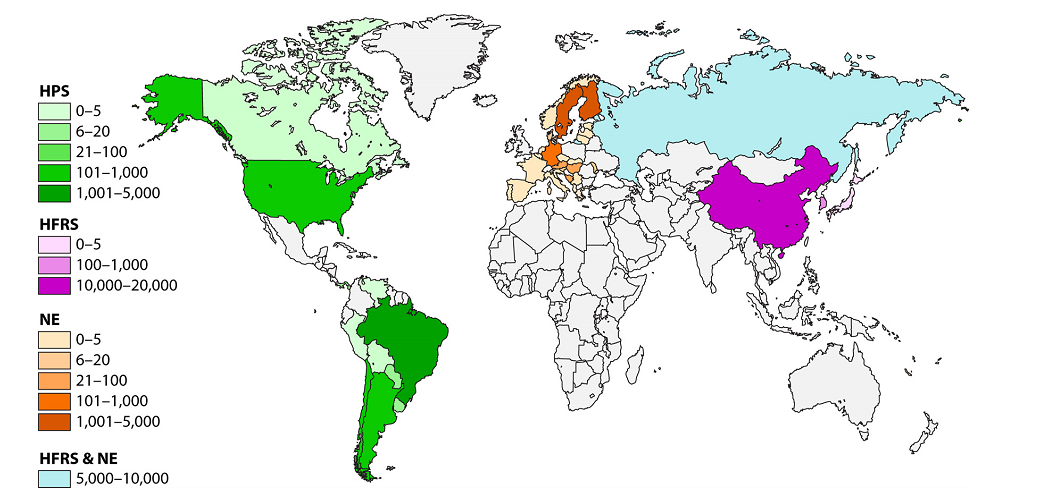
Geographic DistributionHantaviruses occur worldwide, but the distribution of each virus is limited by the geographic range of its reservoir host(s). Species known to be hantavirus carriers may or may not be infected in a given region. The hantaviruses in the Eastern Hemisphere are usually associated with HFRS. Seoul virus and Tula virus can be found in both Europe and Asia, while Dobrava-Belgrade and Puumala viruses circulate in Europe, and Hantaan, Amur-Shoochong, Gou, Thailand and Thottapalayam viruses occur in Asia. There are reports of Puumala or Puumala-like viruses in rodents in Asia. Sangassou, Bowe and Uluguru viruses occur in Africa. There is currently no evidence for hantavirus-associated disease in Australia, although seropositive rodents have been reported. Table: Hantavirus types, their hosts, Distribution and disease associationsThe most important hantaviruses causing HFRS are Hantaan virus, Puumala virus, Dobrava virus and Seoul virus. Other hantaviruses such as Amur virus are also associated with this disease. HFRS includes several diseases that formerly had other names, including Korean hemorrhagic fever and epidemic hemorrhagic fever. ”Nephropathia epidemica (NE)” is sometimes used for a mild form of HFRS, which is often caused by Puumala virus or Saaremaa virus. Hantavirus pulmonary syndrome is caused by a number of hantaviruses in North and South America. In the United States and Canada, the Sin Nombre virus (with its Monongahela and New York variants) is responsible for most cases. HPS can also result from infection by the Muleshoe, Bayou, and Black Creek Canal viruses, as well as other named or unnamed hantaviruses. In South and Central America, Andes virus and its variants are important causes of HPS; Choclo, Castelo Dos Sonhos, Juquitiba, Bermejo, Maciel and other hantaviruses can also cause this syndrome. Some hantaviruses have yet been not been linked to human disease, either because they are not pathogenic for humans or because their rodent hosts are unlikely to pass the virus to humans. Figure: Geographic distribution of approximate hantaviral disease incidence by country per year Incubation PeriodThe incubation period for HFRS can range from approximately one to 6 weeks, while incubation periods of 1-7 weeks have been reported in HPS. Many cases of HFRS and HPS seem to become apparent in about 2-3 weeks. Prevention • Keep mice and rats out of your home. • Clean up mouse and rat urine, droppings, and nesting materials with a disinfectant or a mixture of bleach and water. Hantaviruses are susceptible to many disinfectants including 1% sodium hypochlorite, 70% ethanol, 1-5% peracetic acid, A 10% sodium hypochlorite solution has been recommended for heavily soiled areas. Viruses in solution can be inactivated by heating to 56°C (133°F) for at least 15 minutes. Dried viruses were reported to be inactivated by 2 hours at 56°C. Treatment There is no specific treatment, cure, or vaccine for hantavirus infection. If infected individuals are recognized early and receive medical care in an intensive care unit, they may do better. In intensive care, patients are intubated and given oxygen therapy to help them through the period of severe respiratory distress. The earlier the patient is brought in to intensive care, the better. If a patient is experiencing full respiratory distress, it is less likely that the treatment will be effective. Diagnostic Tests HFRS and HPS are often diagnosed by serology. Antibody titers can usually be detected by the time the clinical signs develop, or soon afterward. Specific IgM or a rise in the IgG titer is diagnostic. ELISAs, immunochromatographic tests and immunofluorescent antibody tests (IFA) are the most commonly used serological tests, but other assays, including immunoblotting and virus neutralization, may also be available. Virus neutralization can distinguish serological reactions to different rodent-borne viruses, but the requirement for live virus limits its use. Antibodies to the hantaviruses carried in insectivores and bats may not be detected with the currently used serological tests. Clinical cases can also be diagnosed by detecting antigens in tissues with immunohistochemistry, or viral RNA in blood, saliva and tissues with RT-PCR. Some PCR tests use species-specific primers, but tests that can detect multiple hantaviruses have also been published. Nucleic acids may not be found in some patients by the time the symptoms develop. Conversely, one study detected Andes virus nucleic acids in some household contacts before they developed symptoms or became seropositive. Virus isolation can also be used for a definitive diagnosis; however, this is uncommon, due to the risks associated with culturing these viruses. In addition, some hantaviruses have never been successfully isolated in cell culture. Isolated hantaviruses can be identified by virus neutralization. Morbidity and Mortality Hantavirus outbreaks are often associated with increased rodent populations or environmental factors that promote human exposure to rodents. Clinical cases are reported to be seasonal in a number of areas. For instance, HPS is more common in late spring and early summer in the U.S., while HFRS occurs more frequently in winter and spring in China. Worldwide, approximately 150,000 to 200,000 people are estimated to be hospitalized with HFRS each year. Most of these cases occur in Asia, although several thousand illnesses are reported each year in Europe and Russia. Many of the clinical cases in Europe are caused by Puumala virus and are mild. HPS is also relatively common in some parts of South America; however, it seems to be infrequent in North America, with approximately 11-50 cases/ year reported in the U.S., and 0-13 cases/ year in Canada. The severity of HFRS and HPS varies with the causative virus and the availability and quality of healthcare. Improved diagnosis and supportive treatments have decreased the case fatality rates for some illnesses, compared to historical reports. The case fatality rate for HFRS ranges from < 0.5% or < 1% in nephropathia epidemica caused by Puumala virus or the Saaremaa strain of Dobrava-Belgrade virus, respectively, to 12% in some other Dobrava-Belgrade virus infections. Amur virus infections are also reported to be severe. Currently, the case fatality rate is reported to be approximately 1-2% for HFRS caused by Seoul virus and 5% for cases caused by Hantaan virus. Rates as high as 10-15% were reported for Hantaan virus in the past. HPS is frequently life-threatening, with case fatality rates estimated to range from 25% to 40% for most viruses. Approximately half of all cases are reported to be fatal in parts of Brazil where Araquara and Paranoá viruses are found, which suggests that these variants might be particularly virulent. Conversely, Laguna Negra virus and Choclo virus seem to cause less severe illnesses, with reported case fatality rates of 15% and 10%, respectively. Conclusion The emergence of zoonotic pathogens remains one of the great unsolved mysteries in biology. In the past century, numerous pathogens have emerged and reemerged, with an estimated frequency of one new pathogen every 18 months. Of these new pathogens, the majority have zoonotic origins in wildlife, and many have been RNA viruses such as the hantaviruses, severe acute respiratory syndrome coronavirus (SARS CoV), Ebola virus, Nipah virus, Hendra virus, West Nile virus, and, most recently, the 2009 H1N1 swine flu that initially emerged in Mexico. These and many other viruses harbored in vertebrates and invertebrates will continue to provide potential sources of new infections of humans and domestic or wild animals. There are many principles that have been learned from past epidemics and pandemics. Fundamentally, however, there remain gaps in our understanding of the ecology and natural history of zoonotic viruses; how they are maintained in their reservoirs; the processes and mechanisms that lead to transmission, host switching, recombination, and reassortment; and molecular events that lead to the transfer and adaptation to a new host and posttransfer adaptation. Gentaur offers many products for the study and diagnosis of hantavirus, check our products here:
0 Comments
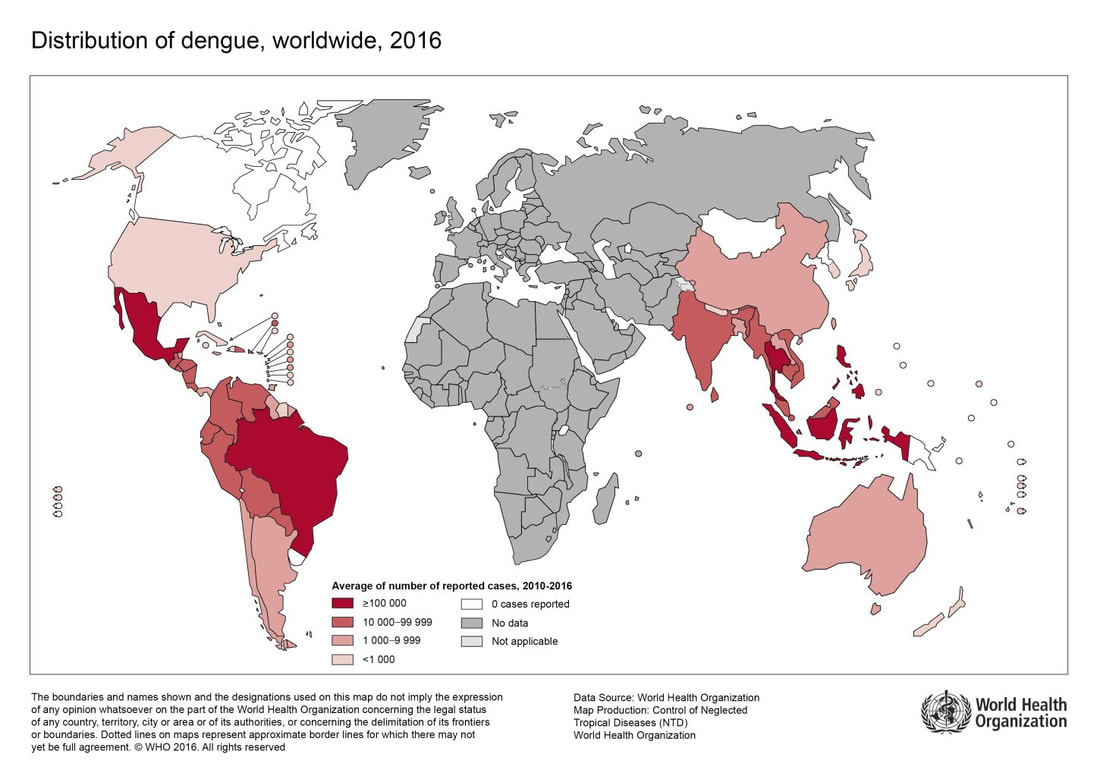
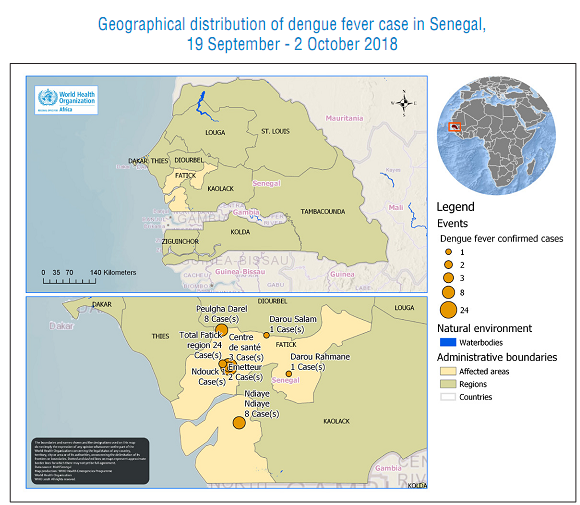
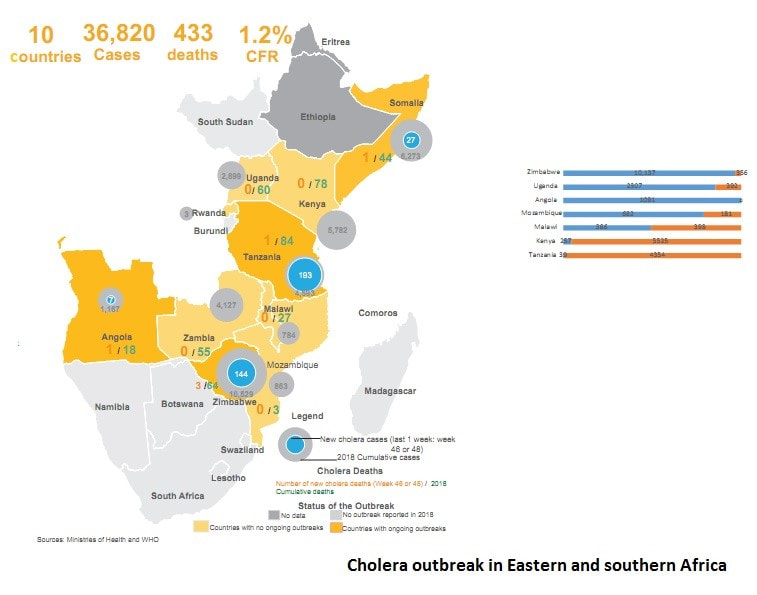
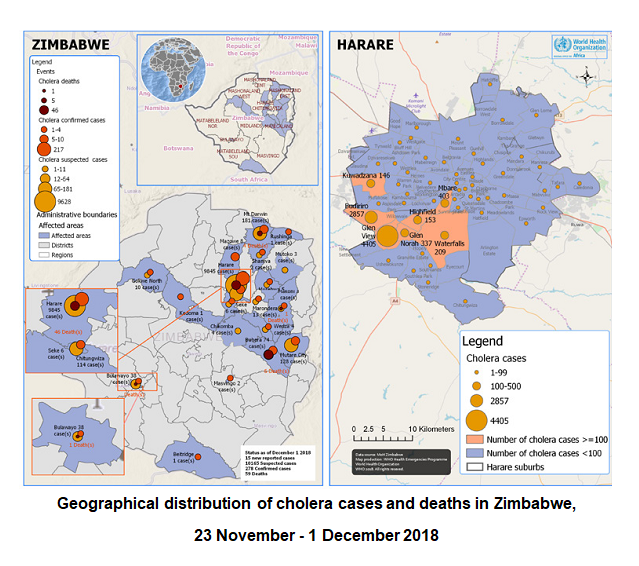
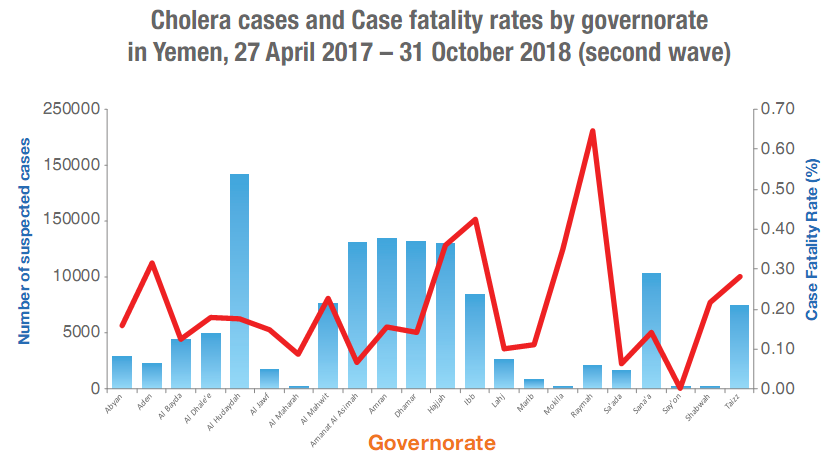
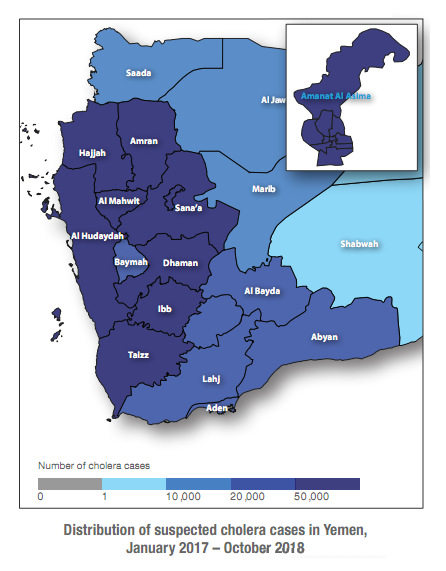
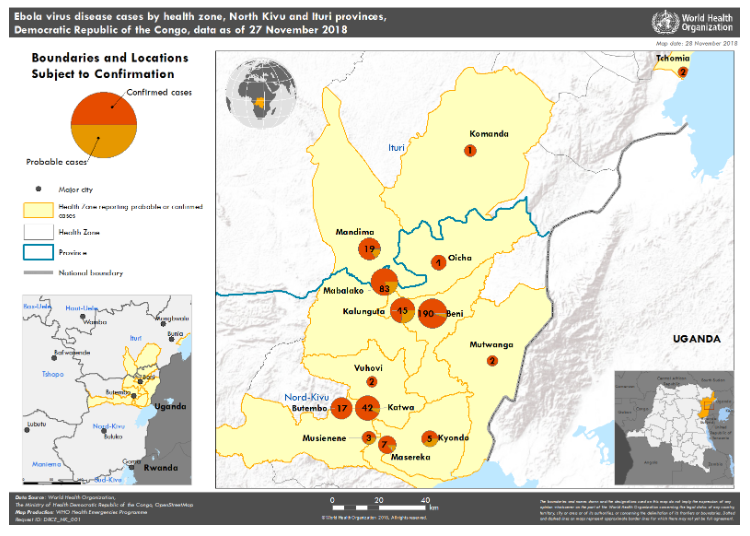
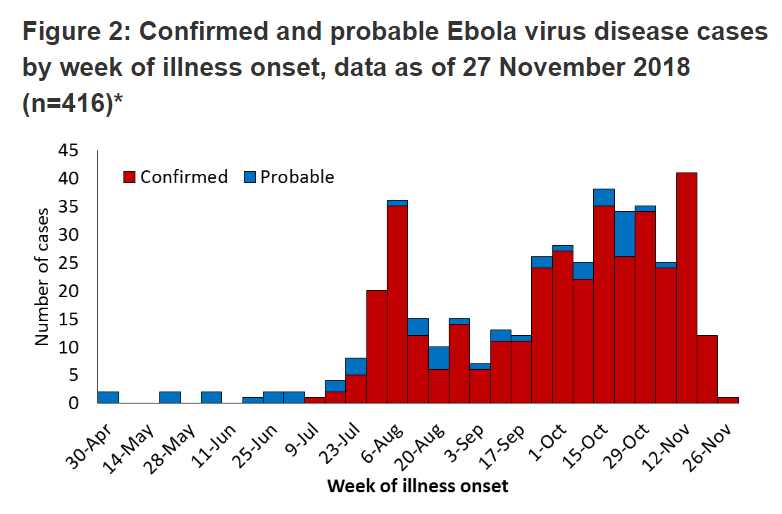
by Houssem Djeridi Salmonella is a genus of bacteria that are a major cause of foodborne illness throughout the world. The bacteria are generally transmitted to humans through consumption of contaminated food of animal origin, mainly meat, poultry, eggs and milk. The symptoms of Salmonella infection usually appear 12–72 hours after infection, and include fever, abdominal pain, diarrhoea, nausea and sometimes vomiting. The illness usually lasts 4–7 days, and most people recover without treatment. However, in the very young and the elderly, and in cases when the bacteria enter the bloodstream, antibiotherapy may be needed. Last few days, a new, huge recall of beef added to the seemingly endless numbers of contaminated food recalls over the past few years. Europe The scale of a Salmonella outbreak in France linked to raw milk cheese has jumped to more than 80 possible cases. Santé publique France, the national public health agency, said 83 people had been identified so far in the Salmonella Enteritidis outbreak, which is up from 14 in the initial announcement. The cheese was also distributed to Austria, Belgium, Germany and Italy. Belgium and Germany have issued recall notices. Authorities in Belgium have warned that certain meat products could be contaminated with Salmonella following processing of potentially contaminated raw materials from the Netherlands. The Federal Agency for the Safety of the Food Chain (FASFC) said an alert through the Rapid Alert System for Food and Feed (RASFF) shows fresh meat used as raw material that could be contaminated with Salmonella Goldcoast was delivered to Belgium from the Netherlands. This RASFF alert covers a suspected foodborne outbreak caused by pig meat from the Netherlands. As well as Belgium, 14 other countries received pig meat products. These are Austria, Canada, Croatia, Cyprus, Denmark, France, Germany, Greece, Italy, Luxembourg, Poland, Romania, Spain and the United Kingdom. The European Commission’s Rapid Alert System for Food and Feed has issued an alert of a foodborne outbreak of Salmonella Goldcoast suspected to be linked to the consumption of pork products from a single slaughterhouse in the Netherlands. Singapore The Agri-Food & Veterinary Authority of Singapore (AVA) has confirmed that there are imports of the implicated frozen raw pork products. AVA is working with importers to remove the implicated frozen pork consignments from the market. The recall is ongoing. Raw meat, including pork, is known to potentially carry bacteria, which may include Salmonella, said AVA. USA Arizona food company JBS Tolleson Inc. is recalling more than 12 million pounds of beef that might be contaminated with salmonella. Eighty-seven more people have been sickened with salmonella linked to recalled beef products, 333 people nationwide have been reported as ill with the outbreak since illnesses began in August. As of December 12, 2018, 333 people infected with the outbreak strain of Salmonella Newport have been reported from 28 states.Illnesses started on dates ranging from August 5, 2018 to November 9, 2018. 91 people have been hospitalized. No deaths have been reported. Food Safety and Inspection Service advices consumers who have purchased these products are urged not to consume them. These products should be thrown away or returned to the place of purchase. Consumption of food contaminated with Salmonella can cause salmonellosis, one of the most common bacterial foodborne illnesses. The most common symptoms of salmonellosis are diarrhea, abdominal cramps, and fever within 12 to 72 hours after eating the contaminated product. The illness usually lasts 4 to 7 days. Most people recover without treatment. In some persons, however, the diarrhea may be so severe that the patient needs to be hospitalized. Older adults, infants, and persons with weakened immune systems are more likely to develop a severe illness. Individuals concerned about an illness should contact their health care provider. The routine detection of Salmonella in foods is an important part of public health because the presence of Salmonella in food can cause health problems. Gentaur offers you many products for the detection of Salmonella in food and other samples. Check our products here :by Houssem Djeridi Dengue is a mosquito-borne viral infection, usually transmitted by Aedes aegypti mosquitoes. The infection causes flu-like illness, and occasionally develops into a potentially lethal complication called severe dengue. The global incidence of dengue has grown dramatically in recent decades. About half of the world's population is now at risk. Dengue is found in tropical and sub-tropical climates worldwide, mostly in urban and semi-urban areas. Severe dengue is a leading cause of serious illness and death among children in some Asian and Latin American countries. In 2018, dengue has been reported from Bangladesh, Cambodia, India, Myanmar, Malaysia, Pakistan, Philippines, Thailand, and Yemen. Recently dengue virus outbreak has been reported in Cuba, according to Cinco de Septiembre, official newspaper of Cienfuegos in south central Cuba. This type of dengue has not been reported in Cuba since 1977. "A new epidemic of dengue has broken out, causing alarm and clinical developments, but luckily we have not had to mourn the loss of life up until now," the newspaper quoted provincial health director Salvador Tamayo Muniz, speaking to regional leaders. The last time this form of dengue was active in Cuba, more than 500,000 people from the eastern area of the island became infected. In Africa, dengue virus is not well recognized, On 27 September 2018 an investigation has been instituted in Senegal and it identified 180 cases that met the dengue fever case definition; of these 120 were investigated. Blood specimens were collected from suspected cases, an additional 21 cases among symptomatic patients tested positive for dengue fever by polymerase chain reaction (PCR). Further analysis carried out by the Institute Pasteur Dakar show a circulation of dengue fever virus serotype 1 (DENV-1). Dengue infection is cause by four serotypes; DEN-1, DEN-2, DEN-3, and DEN-4, each one of these viruses has different interactions with the antibodies in human blood serum. There is no specific treatment for dengue/ severe dengue, but early detection and access to proper medical care lowers fatality rates below 1%. Laboratory diagnosis is carried out by virus isolation, demonstration of viral antigen, presence of viral nucleic acid, and antibodies. Further, recombinant dengue envelope protein can be used to detect specific antibodies, both IgG and IgM against all four serotypes of virus using an E. coli vector. The purified protein can then be used for detection of dengue specific IgG or IgM antibodies in patient serum with higher sensitivity and specificity, than that of traditional assays. Molecular detection can be accomplished by a one-step, single-tube, rapid, multiplex, RT-PCR for serotype determination. Despite many advantages of the modern techniques, isolation of virus is still considered as "gold-standard" in dengue diagnosis. Gentaur offers many products for the identification and the control of dengue virus contaminations, check out our products here :by Houssem Djeridi Cholera is an acute diarrhoeal infection caused by the bacterium Vibrio cholerae, infecting people most often via contaminated water or food. Every year, cholera causes an estimated 3 to 5 million cases, and 100,000 to 120,000 deaths. The short incubation period (2 hours to 5 days) enhances the potentially explosive pattern of outbreaks. Cholera affects both children and adults and can kill within hours if untreated. it can kill especially those with weakened immune systems within hours if left untreated. Many cases of cholera have been reported in 2018 in different countries: 5 October 2018 (Zimbabwe), 5 October 2018 (Niger), 20 September 2018 (Zimbabwe), 14 September 2018 (Algeria), 14 June 2018 (Cameroon), 29 March 2018 (Somalia), 2 March 2018 (Kinshasa, Democratic Republic of the Congo), 19 February 2018 (Mozambique), 12 January 2018 (United Republic of Tanzania)… In Africa 10 countries have reported more than 36,820 cholera/AWD cases and 433 deaths (Case Fatality Rate, 1.2%), since the beginning of 2018. These countries are: Zimbabwe, Angola, Mozambique, Rwanda, Kenya, Malawi, Somalia, Tanzania, Uganda and Zambia. Zimbabwe, Angola, Tanzania and Somalia have ongoing cholera outbreaks. According to an analysis in seven countries (Angola, Kenya, Mozambique, Malawi, Tanzania, Uganda and Zimbabwe); more cholera cases emerge from urban areas as compared to rural areas. urban areas account for 57.1% (14,899 cases) of the total caseload while rural areas account for 42.9% (11,206 cases) An increase in the epidemic has been noted in Zimbabwe, new cases were reported from Harare (50) and Mt. Darwin district in Mashonaland Central (94 including 3 deaths). Cumulatively, a total of 10,529 cases including 64 deaths have been reported in 2018. The cumulative number of suspected cholera cases reported in Yemen since October 2016 is 1 308 069 including 2 725 related deaths with a case fatality rate of 0.21%. The country experienced a second wave of this outbreak from 27 April 2017. The total number of reported cases of suspected cholera is 1 282 242 including 2 596 related deaths with a case fatality rate of 0.20%, was reported during the second wave. Watery diarrhea can be helpful in identifying cholera because of the rapid spread of the disease. But it is impossible to identify the cholera without testing stool samples, so it is very important to identify cholera because of the potential for a widespread outbreak, For the diagnosis of cholera in laboratories; Gentaur offers kits to isolate and identify Vibrio cholerae serogroup O1 or O139. Check our products here Gentaur povides kits and reagents to isolate and identify Vibrio cholerae serogroups O1 and/or O139 for laboratory diagnosisby Lieven Gevaert and Djoumana Ounas Since 21 November 2018, 36 new cases have been reported: 13 in Beni, 9 in Katwa, 6 in Kalungunta, 6 in Butembo, 1 in Kyondo and one in Oicha. Two health workers from Katwa and Kyondo were among the newly infected. 42 health workers have been infected so far. Twelve other survivors were released from Ebola treatment centers in Beni and Butembo and reintegrated into their communities. The risk of spreading the epidemic in other provinces of the Democratic Republic of Congo, as well as in neighboring countries, remains very high. During the past week, alerts have been reported in South Sudan and Uganda. EVD has been excluded for all alerts to date. Check Gentaur Genprice products related to the identification and the detection of Ebola Virus
Also in 2018, Gentaur Genprice Explores All Facets of the Global Market for Biotechnology and Laboratory Products at the Düsseldorf Exhibition Center and Will Find Answers to all Questions Asked by its Customers. This International Event Will Unveil a New Range of Unique Novelties to the Research and Diagnostic Worlds. |
Genprice Inc. USA
(718) 513-2983
[email protected]
Gentaur SRL Italy
02 36 00 65 93
[email protected]
Gentaur GmbH Germany
+49 0241 40 08 90 86
[email protected]
Gentaur Ltd. UK
020 3393 8531
[email protected]
Gentaur Spain
0911876558
[email protected]
Gentaur Sarl France
01 43 25 01 50
[email protected]
Gentaur BV Netherlands
0208-080893
[email protected]
Gentaur BVBA Belgium
0032 265 09 23
[email protected]
Gentaur Sp. z o.o. Poland
058 710 33 44
[email protected]
(718) 513-2983
[email protected]
Gentaur SRL Italy
02 36 00 65 93
[email protected]
Gentaur GmbH Germany
+49 0241 40 08 90 86
[email protected]
Gentaur Ltd. UK
020 3393 8531
[email protected]
Gentaur Spain
0911876558
[email protected]
Gentaur Sarl France
01 43 25 01 50
[email protected]
Gentaur BV Netherlands
0208-080893
[email protected]
Gentaur BVBA Belgium
0032 265 09 23
[email protected]
Gentaur Sp. z o.o. Poland
058 710 33 44
[email protected]